
2024
“Yeyasso: the cooperative where all hopes are allowed”
The Yeyasso cocoa and coffee cooperative in the Ivory Coast makes every effort to stay one step ahead of major market trends
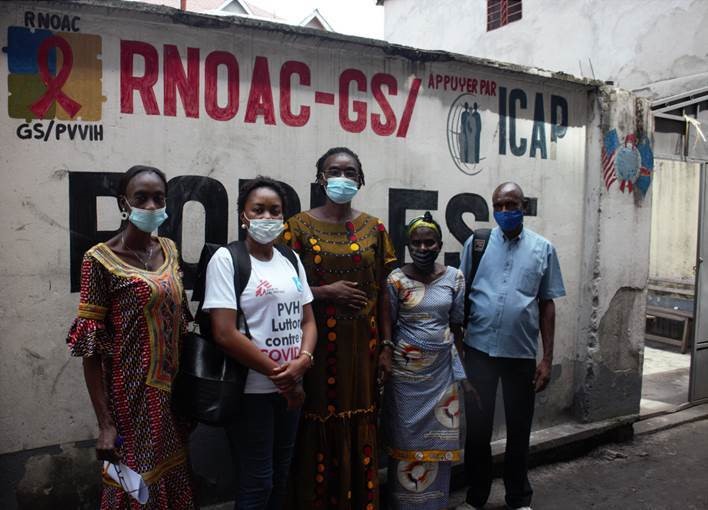
Read articleFor five years, the King Baudouin Foundation has been pooling funds from some fifteen Funds it manages – almost 200,000 euros per year – to reinforce their impact in supporting the fight against HIV/AIDS by healthcare workers and volunteers in Kinshasa, with support from MSF Belgium. In addition to the work done at the hospital, patients are also cared for at community medicine distribution posts (PODIs), where they treat the disease as well as fight the stigmas, in an effort to fight the rejection endured by those who have contracted the virus.
“AIDS patients are still victims of stigmatisation and rejection. In the PODI premises, patients can talk with other members of the community without embarrassment.”
Jean Lukela, founder of the national network of community-based organisations for AIDS sufferers
 Dr Gisèle Mucinya is the Medical Director of the MSF’s project to fight HIV/Aids in Kinshasa. She manages the Kabina Hospital Centre (CHK), which is a referral centre in the DR Congo for the care of people living with HIV/AIDS, as well as a number of health units across the city. She explains what difficulties impede access to screening and care.
Dr Gisèle Mucinya is the Medical Director of the MSF’s project to fight HIV/Aids in Kinshasa. She manages the Kabina Hospital Centre (CHK), which is a referral centre in the DR Congo for the care of people living with HIV/AIDS, as well as a number of health units across the city. She explains what difficulties impede access to screening and care.
“We lack antiretroviral (ARV) treatments, and few patients know their viral load. In the DR Congo, half a million people are affected by the illness, although this is thought to be a significant underestimate. It is estimated that the quantity of virus in the blood has been established for only 30% of the patients treated. This low figure is explained by the lack of hospital facilities, the scarcity of available tests and medicines, the complexity of analysing blood samples and the absence of diagnosis of opportunistic infections such as tuberculosis, which is often present among patients with HIV. And the Covid-19 epidemic has not facilitated our work and is perturbing provision of ARVs.” In addition to these issues, there is the lack of information about HIV/AIDS among the general public. “It is estimated that more than half of the people living with HIV/AIDS receive no treatment.”
Many patients come to the CHK as emergencies, when their immune systems have almost collapsed. “Such behaviour can also be explained by the stigmatisation to which AIDS sufferers are subjected, including even in the hospital environment” explains Dr Mucinya. “They are rejected by their families, lose their jobs and are excluded from healthcare, or see their children excluded from school. In people’s minds, HIV/AIDS is often linked to prostitution or a curse. Divorce is widespread among couples where one spouse carries the virus. For the children of contaminated parents, AIDS can lead to a living hell. Orphans of sick parents are often considered as child witches and find themselves on the streets alongside Kinshasa’s street children. This fear of abandonment leads those who are ill to stay quiet for as long as possible: they resign themselves to going to hospital when it’s too late.”
At the CHK, treatments related to HIV are free of charge because they are partially paid for by MSF. Treatment is supposed to be free in all health facilities in the DR Congo, but as healthcare in general is largely under-financed, patients with HIV/AIDS are asked to dip into their own pockets. This is a sacrifice that most people, surviving on less than two dollars a day, can hardly do.
The crusade against AIDS is not confined to the corridors of the CHK. With support from MSF – which itself benefits from support from several Funds managed by the King Baudouin Foundation – 13 community medicine distribution posts (PODI) were set up some ten years ago. There are nine of these posts in Kinshasa and four others in the provinces. The objective is to provide screening, antiviral treatment and re-establishing contact with patients who have been lost to follow-up. In the PODI, you don’t see medical personnel, but rather members of the community. They are places where information is exchanged about HIV/AIDS and the prejudices it generates with the aim of fighting the rejection that weighs so heavily on those who have contracted the disease. Numerous young people also work in clubs that have recently been created for them and where they distribute ARVs to other adolescents who have become their confidants.
Numerous volunteers who work in the PODI themselves carry the virus. In his role as founder of RENOAC, the national network of community-based organisations for AIDS patients, Jean Lukela manages most of these centres. He explained “I was a patient at the CHK and I have been receiving antiretroviral treatment since 2003. I asked myself how we could fight this disease. I created support groups to provide answers to the most basic questions: how medicines be should taken, how to interpret results, overcome family and social problems caused by the disease and obtain financing. We fought to become independent and to move away from the status of patients and thus weaklings to which we were confined.”
Ten years after opening the first PODI, the experience was extended to beyond the Congolese capital. And this yielded positive results: treatments are followed-up, patients are responsible and there is less fear about admitting to symptoms than in a traditional healthcare setting. However, economic problems render the existence of these patients very difficult and fear of Covid-19 has led to a pause in the organisation of screening sessions and awareness building.
Papa Jean was the first patient of the first PODI, which was clandestine at the time. Today, he supervises the PODI East team. He remembers, “At the beginning, we wondered how we could begin and with whom. MSF had already tried to set up the first decentralised premises in a health centre, but the patients came back to CHK. In 2004, I joined a support group, to see how other patients were involved in the battle, how they expressed themselves and that gave me the desire to get involved. If we don’t get involved, who is going to do it for us? This activism encouraged me. It was that group that initiated us in how to do things, at first clandestinely. I know that, today, we can save lives through our testimonies.”
More about support for the King Baudouin Foundation
Since 2016, the annual contributions (of almost 200,000 euros a year) from some fifteen or so philanthropic funds managed by the King Baudouin Foundation reinforce the work done by MSF Belgium and its partners. The objective is to win the battle being waged by NGOs against HIV/AIDS in the DR Congo together with the country’s healthcare professionals and volunteers (patients).

2024
The Yeyasso cocoa and coffee cooperative in the Ivory Coast makes every effort to stay one step ahead of major market trends
Read article
2023
A grant from BPF has dramatically boosted a young entrepreneur’s aim of radically improving the lives of girls and women in Rwanda by producing eco-friendly, reusable, and hygienic sanitary pads.
Read article
2023
One in two children in South Kivu is chronically malnourished. Kesho Congo is developing software to monitor patients more closely and using data research to find solutions to this complex problem.
Read articleTo stay informed about news from our partners and new calls for proposals
Subscribe to the newsletter